ivermectin has been paid tens of millions of dollars by US insurers despite little evidence that it works to treat or prevent the illness. According to the new study, private and Medicare insurance plans spent over 2.5 million dollars for covidy prescriptions in a single week in August of 2021.
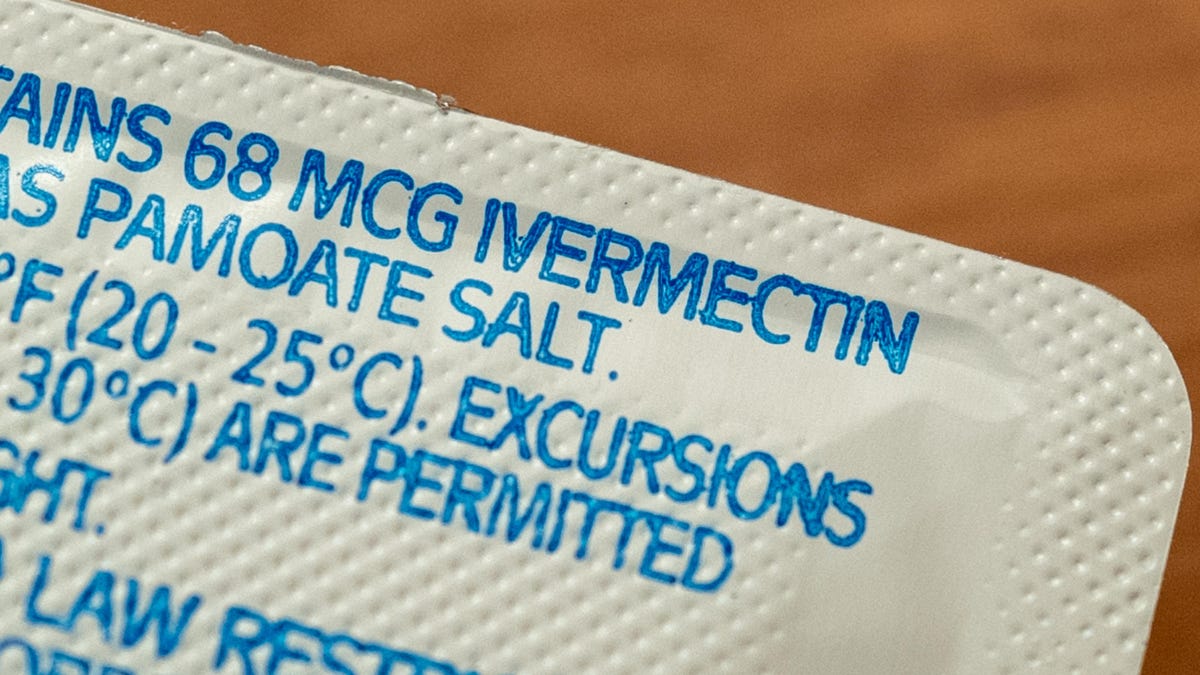
Ivermectin has been used in wide use for over 40 years. It was one of the drugs that received a second look as a possible treatment for covid-19 based on early lab results. The field of covid-related research on ivermectin has been plagued with poor quality data and allegations of widespread fraud over the past two years. There are still important ongoing studies of ivermectin for covid-19, but the largest and most rigorous trials to date have found no clear benefit for the drug in either treating or preventing covid-19.
ivermectin is still being used as a covid treatment by some people and doctors despite the lack of evidence. These devotees tend to be politically right-wing, and they often have unsupported claims about the dangers of vaccines. They stock up on drugs like ivermectin to seem to stay safe, but they downplay the harms of the epidemic.
In the U.S., ivermectin use has risen even though no public health authority has recommended it. India made ivermectin widely available for treatment, though health authorities there stopped endorsing it because of the lack of evidence. Researchers at the University of Michigan Medical School and Boston University don't know how much the added and likely wasteful use has cost.
The team analyzed prescription claims from a de-identified database of over 6 million customers on either private insurance or Medicare Advantage plans. They focused on claims made during the week of August 13, 2021. They used the data to estimate how many people were prescribed ivermectin for covid-19.
They estimated that almost 85,000 covid-related ivermectin prescriptions were given out to Americans on private and Medicare Advantage plans that week. Out-of-pocket costs for customers of Ivermectin ranged from $22.48 for privately insured patients to $13.78 for Medicare Advantage patients. The net total spending was $2,493,716.
The authors wrote that the findings suggest that insurers subsidized the costs of ivermectin prescriptions for covid-19 even though economic theory holds that insurers should not cover ineffective care.
The cost of covid-related ivermectin would have reached $129.7 million if extrapolated to a whole year, but it is not certain if the trends would have stayed the same. It is possible that the study is underestimating the financial toll since they weren't able to look at Medicaid spending. Some states began to investigate doctors who prescribed ivermectin last year, and this may have led patients to seek the drug elsewhere. The authors say that if the yearly estimates are accurate, it would eclipse other forms of wasteful spending in medicine, such as the use of unneeded diagnostic testing for lower back pain.
The authors conclude that insurers should look into restricting the use of covid-19 drug, since it probably doesn't work and the amount of money spent on it is probably excessive. This would make it mandatory for any prescription of the drug to be approved by the insurer first.
The use of ivermectin for non-covid-19 indications is not impeded by these restrictions. The number of patients who would experience barriers to evidence-based treatment for ivermectin would be small if the restrictions were in place.