The image is from thecdn.vox-cdn.com.
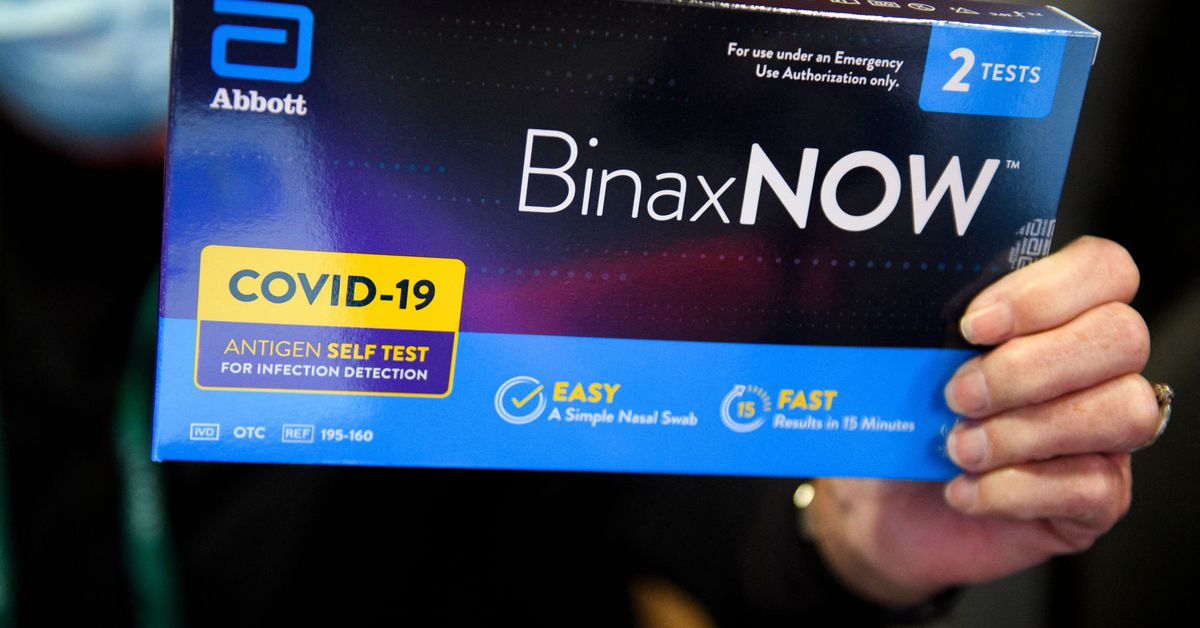
The Biden administration announced a policy on Monday that will require insurance companies to reimburse up to eight over-the-counter at- home COVID-19 tests for their customers, as first reported by the Associated Press. The administration said that the update is part of a larger plan to increase access to COVID-19 testing.
Under the new policy, insured Americans will either have to purchase the test kits under their insurance or submit receipts to their insurance for reimbursement. A family of four with the same plan can be reimbursed for up to eight COVID tests per month. Consumers will be required to do more work under the plan.
The US Department of Health and Human Services said in a Monday statement that the plan incentives companies to cover upfront costs and makes it easier for privately insured consumers to go online or to their local pharmacy or store to purchase a test.
The update comes nearly a month after the administration announced that it was working with Google to release a website to distribute 500 million free COVID-19 tests to Americans, a plan that came in the midst of a mass testing shortage in the US and the spread of the omicron variant. The website has not yet been launched.
The White House said at the press conference that Americans should be able to order tests online later this month, but there are several components involved in manufacturing and distributing the tests that could cause further delays.