In mice, researchers found compelling evidence that Alzheimer's disease could be caused by a blood-to brain pathway.
Although this work is still in its early stages and cannot be applied to humans yet, it is a promising lead that could help us understand why the degenerative diseases have been so difficult to treat.
The protein fragment beta-amyloid has been portrayed as the main villain in Alzheimer's disease development over the years by decades of detective work.
Despite its popularity, we still don't know much about the short chain of amino acid and its role in the body. We do know that if it forms clumps inside the brain, the prognosis for long-term mental health is not good.
However, the case against beta-amyloid doesn't seem to be very clear.
Recent research has revealed a lot about the movement of beta-amyloid plaques throughout the body, and into the brain. It also plays a role in the eventual death of neurons. There are still questions, like why beta-amyloid plaque therapies don't work as expected.
A continuing area of interest is not the plaques, but the relationship beta-amyloid and a class fat-carrying chemicals called Lipoproteins.
Researchers from Australia's Curtin Health Innovation Research Institute discovered compelling evidence that beta amyloid proteins are being smuggled into brains via the lipid transport system.
John Mamo, a physiologist and lead investigator in this study, says that toxic protein deposits in Alzheimer's patients' brains are likely to be caused by fat-carrying proteins in blood.
"This 'blood to brain pathway' is important because if we manage the levels of lipoprotein-amyloid in the blood and prevent them from leaking into the brain, it opens up new possibilities for treatments to slow down memory loss and prevent Alzheimer's disease."
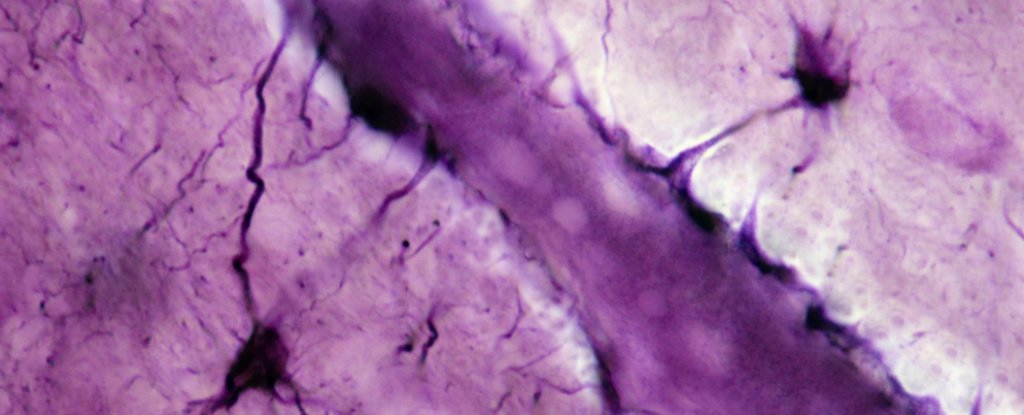
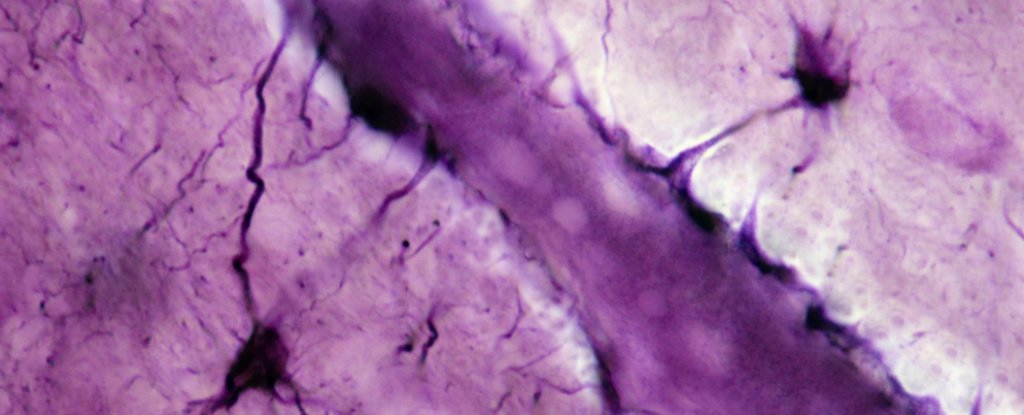
Researchers have struggled to figure out how small proteins accumulate in brain cells, eventually leading to their death.
It could be that it is simply made in large quantities within the brain's tissues. However, having high levels of beta-amyloid within the peripheral blood is a good indicator of brain plaque development later.
One clue is found in the way that a soluble low-density protein can remove about 70-90 percent of beta-amyloid from human plasma. The blood vessels are also damaged by the fat-carrying complex that leaks from the capillaries deep within Alzheimer's brains.
Studies on mice further confirmed the existence of a link between lipoproteins, beta-amyloid and subsequent studies. For example, rats fed high levels of saturated fats had the same leaky blood vessels as humans.
However, it is possible that beta-amyloid could have been produced in the brain in toxic levels. Mamo and his colleagues engineered mice to express genes that build beta-amyloid in the liver.
This way, any Alzheimer's-like pathology that they detected in the brains of the mice models had to be caused by beta-amyloid being brought in from the outside.
Mamo says, "As we expected, the study found lipoprotein-amyloid production in mouse models suffered inflammation in their brains, accelerated brain cell loss, and memory impairment."
Although there is still much to be discovered, this discovery suggests that there may be treatments for Alzheimer's disease that target diet or that use pharmaceuticals to control how beta-amyloid interacts with lipoproteins.
The number of people suffering from Alzheimer's disease will rise as the world's population ages. Currently, the condition affects more than 30,000,000 people.
We can learn more about beta-amyloid's movement through our bodies and find early treatments to treat or prevent neurological dysfunction that affects so many people.
This research was published by PLOS Biology.