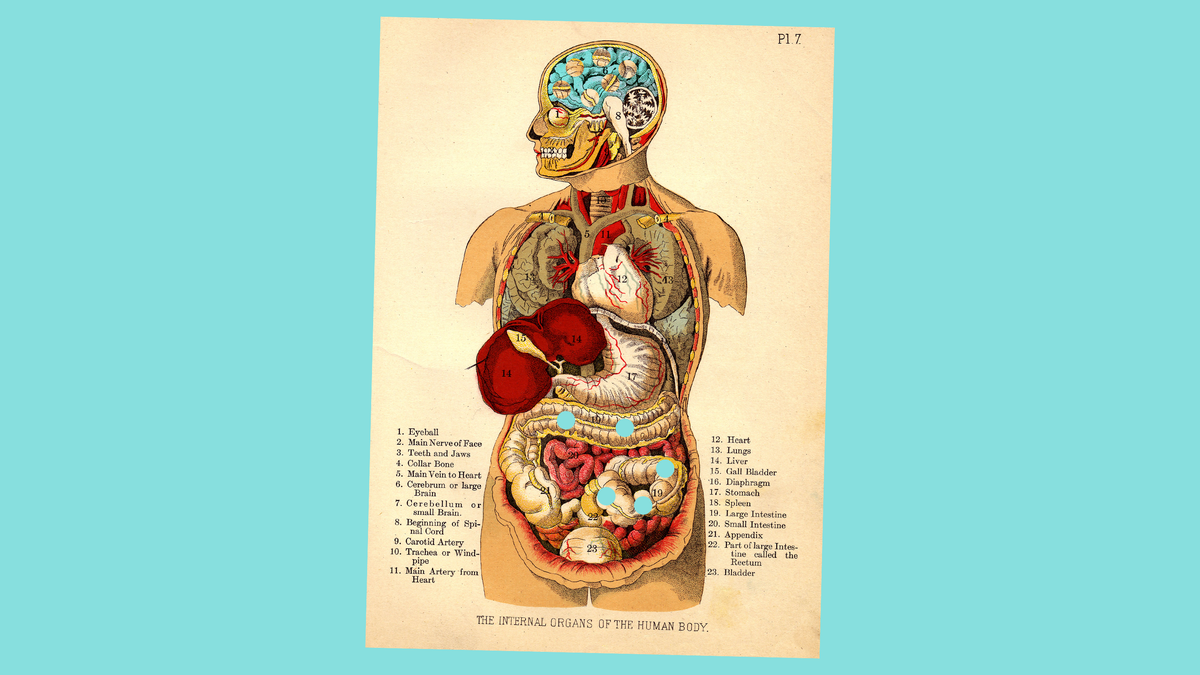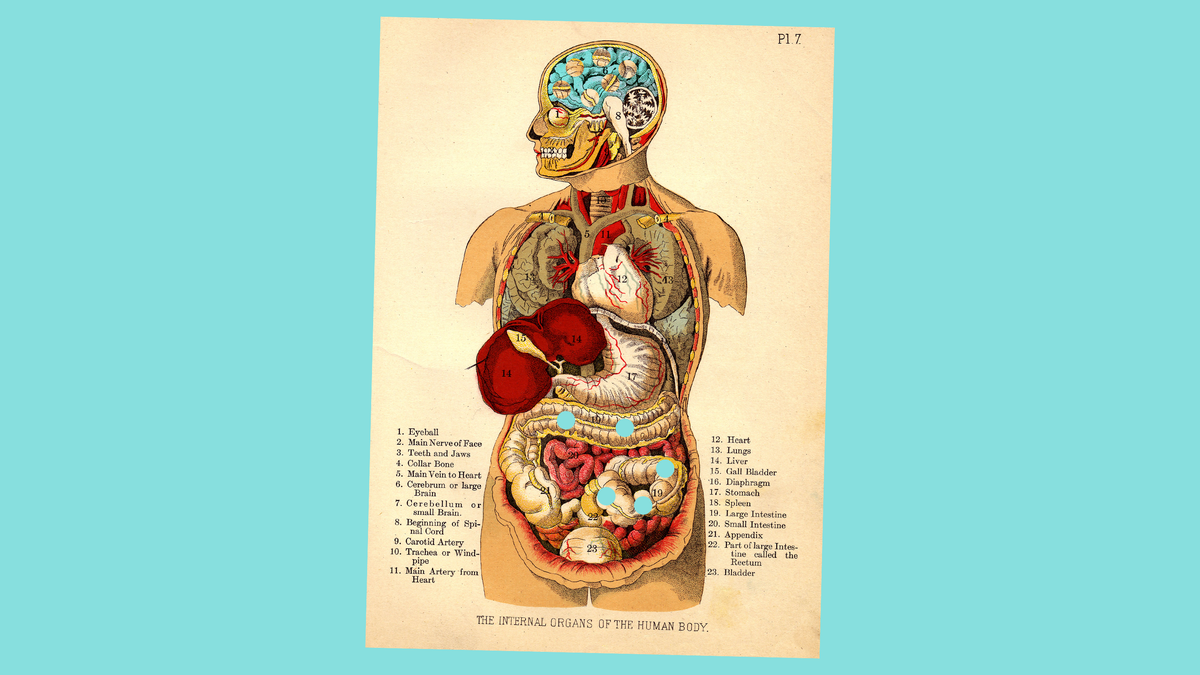
Our guts are home to trillions of microorganisms. These germs can affect digestion, immune system and brain function. Scientists are also investigating the role of gut bacteria in neurodegenerative and psychiatric conditions like Alzheimers and Parkinsons. This could help to identify the causes of these diseases earlier and provide new treatment targets if gut microbes are found to be influential.
Advertisement
Neurodegenerative diseases cause nerve cells to gradually die, leading to problems in movement or mental function. These diseases have become more common over the last 30 years due to an aging population. However, there is no cure and very few effective treatments. Millions of people are affected by Parkinson's and Alzheimer's diseases.
These diseases are caused by a combination of environmental, genetic, age-related, lifestyle, and genetic factors. Doctors can't usually pinpoint the cause. Scientists are now increasingly interested in the role of microbes in the gut because the brain is connected to the gut.
This research has mainly focused on Parkinsons disease, which is often associated with digestive problems. However, preliminary connections between the gut microbiome (and other neurodegenerative diseases like Alzheimers or amyotrophic lateral sclerosis) are beginning to emerge.
Bacteria make up the majority of microorganisms found in our stomachs. They are in direct and indirect communication to the nervous system. This controls movement, mental functions, and automatic processes such as breathing.
Our microbes may be communicating with the brain through a two-way link called the gut-brain-axis. This involves nerves and chemical pathways. Gut bacteria is capable of synthesizing neurotransmitters, brain molecular messengers and other chemicals. These molecules can travel to brainstem if they are absorbed through the gut walls and into bloodstream. These bacteria can also interact with immune cells. This interaction could cause brain damage through immune cell signaling pathways or directly, in the case of late neurodegenerative diseases. It is possible for immune cells to infiltrate the brain through the bloodstream and more porous blood vessels during the later stages of the disease.
This leads to the big chicken-and/or-the-egg problem. Is it possible that the disease caused the microbiome's to change or did the disease influence the microbiome?
Advertisement
Research into the role of gut bacteria and neurodegenerative diseases remains a new field. Timothy Sampson assistant professor of physiology, Emory University, stated that there is some legitimate skepticism.
This field is still relatively new, so there are many unknowns. Jan Pieter-Konsman from the University of Bordeaux, a neuroimmunologist, stated that it is still an emerging field. Studies of the gut microbiome in neurodegenerative diseases and their effects on the immune system were limited to comparing the microbial communities between people with and without these diseases. The majority of studies did not look at the operation within these ecosystems.
Advertisement
Maureen OMalley from the University of Sydney, a philosopher of microbiology researcher, stated that you need to dissect this community in order to understand these interactions. In the last five years, however, researchers have been focusing more on these interactions to determine which microbes or molecules may be responsible for disease.
Researchers are particularly interested in Parkinson's disease. People often experience constipation and other digestive issues years before they start to develop movement-related symptoms.
Advertisement
Lynne Barker, an associate professor of cognitive neuroscience at Sheffield Hallam University, stated that one of the most important features of James Parkinson's original diagnosis of shaking palsy (now Parkinsons disease) was the observation of persistent constipation in patients. It is not a secret that Parkinsons disease affects the gut.
To determine the bacteria composition of the gut, scientists examine stool samples for bacterial genes. These studies showed that the microbiomes of Parkinson's patients differ from those who are not. These differences are independent of any other factors, such as diet. Sampson said that this leads to the big chicken-andthe-egg problem. Is it possible that the disease caused the microbiome's to change or the disease itself?
Advertisement
Purna Kashyap (a professor of medicine and physiologicallogy) and his team conducted a preliminary study using mice models of Parkinson's disease. They found that mice need to have gut bacteria in order to develop movement-related symptoms. Movement problems did not occur in germ-free mice. These mice were free from any bacteria, fungi, viruses or other organisms.
Studies in mice and rats have also shown that Escherichiacoli, a gut bacteria, makes proteins similar to the alpha-synuclein protein clusters found in Parkinson's disease brains. Sampson found that mice with an overexpress of alpha-synuclein have movement symptoms and alpha-synuclein accumulation in their brains.
Advertisement
OMalley warned that although these animal studies are more thorough than previous studies, they need to be interpreted with caution as nimal studies can often not replicate in humans. She said that you can still find some suggestive results that will allow you to create a better understanding of what's happening.
A few research groups are now looking into the effects of gut microbiome dysfunctions on other neurodegenerative diseases like Alzheimer's. Alzheimer's patients are affected by protein clumps known as beta-amyloid plaques. These disrupt brain cell function. A role for microbes in the gut is also suggested by mouse models of Alzheimer's disease.
Advertisement
We don't know the brain mechanisms and we won't be able develop effective treatments until we do.
Barbara Bendlin, a University of Wisconsin Madison professor of medicine, stated that mice with fewer germs don't develop amyloid plaques as much if they are kept clean. This does suggest that there is a link between microbes, Alzheimer's disease pathology, and the development of microbes.
Advertisement
Bendlin and her colleagues have used stool samples to determine the gut microbiomes of Alzheimer's patients as a starting point for human research. They found that Alzheimer's patients had less diversity in bacterial populations and higher levels of certain bacteria. This was in a small study with 25 people with Alzheimers disease and 25 without. To find out if there were any relationships between Alzheimers-related biomarkers, they also examined the cerebrospinal fluid (which surrounds the brain, spinal cord, and brain) of participants.
Bendlin said that even in individuals who are not symptomatic, we found relationships between the cerebrospinal fluid biomarkers and the microbiome of their gut. This suggested that perhaps there is a link between brain pathology and gut microbiome that may be present before people get dementia.
Advertisement
Scientists are also exploring the links between gut bacteria, ALS and the progressive death of neurons that power muscles. Eran Blacher, a postdoctoral fellow at Stanford University School of Medicine studying the gut-brain axis, found that ALS symptoms were preceded by changes in the microbiome. Blacher stated that this might be a sign that the disease is causing such changes.
Researchers also discovered that certain bacteria in the gut could produce molecules that alter the symptoms of the disease in mice. The mice were given a probiotic supplement containing that bacteria, which increased levels of the molecule Nicotinamide and improved their symptoms. Nicotinamide is responsible for key chemicals in cellular pathways that scientists believe are involved with ALS. Blacher said that we could alter the disease's progression and manifestation by treating mice with specific bacteria.
Advertisement
Blacher's preliminary results in a small number of human patients support those findings: People with ALS had lower levels in stool samples of bacterial genes required for nicotinamide metabolic activity than people without ALS. Their cerebrospinal fluid and blood also contained lower levels of nicotinamide. Blacher said that it is not possible to cure ALS or change the course of disease progression in humans. Larger follow-up studies may reveal more about the mechanisms behind ALS and identify potential therapeutic targets.
However, it remains a mystery how microbiomes are involved in neurodegenerative disorders. Barkers' group is currently analyzing data from a small feasibility research to determine if administering a common probiotic for Parkinsons patients could alter their microbiome composition and impact quality of life. Barker stated that her team is not focusing on the big picture changes in microbial communities like previous work. Instead, they are focusing on specific bacteria species.
Advertisement
However, research is still far from showing microbiome-based therapies for neurodegenerative disorders. Although probiotics and dietary changes may be helpful in alleviating symptoms, they won't cure these complex diseases. Scientists need to understand how neurodegeneration is caused by gut microbes.
Bendlin stated that we haven't yet discovered the brain-related mechanisms and that until that is known, we won't be able develop effective treatments.
Advertisement
Jackie Rocheleau, a journalist and editor who is freelance from upstate New York. She writes about medicine, neuroscience, and public health. Follow her Twitter @JackieRocheleau