An American man lost his vision in his right eye for 2 days. This case could give us more insight into how SARS/CoV-2 affects our immune system.
A COVID-19 diagnosis was made for a patient in his 70s who complained of a runny nose. He presented to the hospital three weeks later with another set of symptoms.
A team of Columbia University Vagelos College of Physicians and Surgeons from New York reported that the man had been able to recover from the worst of COVID-19. However, he was still suffering from headaches a week later.
Soon, he experienced a loss of vision in his right eye. He was unable to see clearly and could only make small movements. It was also very painful to move with this eye.
Although cases of vision impairment following a SARS/CoV-2 infection are not common, they are not uncommon. There are a few case reports that suggest possible links. This case is notable for the combination of symptoms including intense headaches and discomfort within the eye.
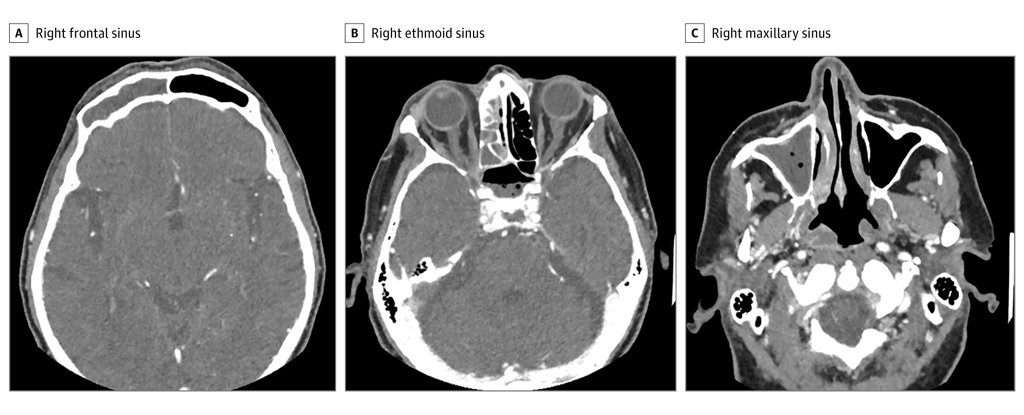
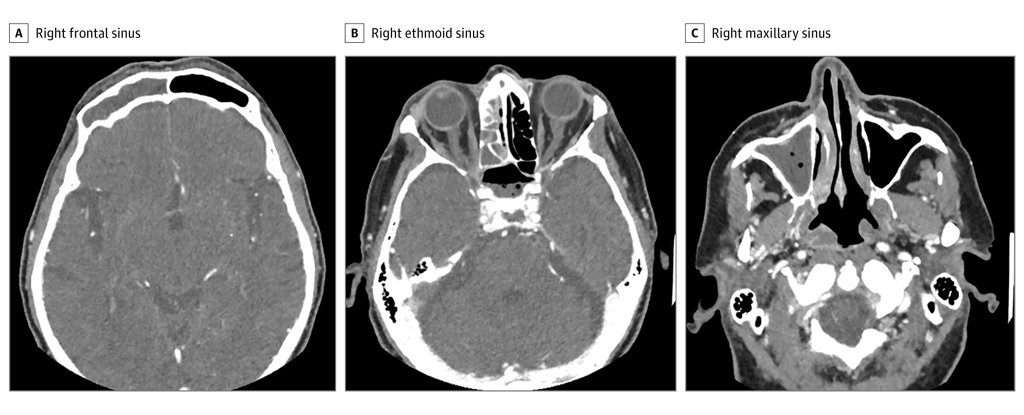
The source of the patient’s pain was quickly identified by a CT scan. It was a severe inflammation of sinuses that ran down his right side. It was so severe that it was causing bone erosion.
At first, the surgery appeared to be a winning strategy. However, the pain soon returned and his vision began to worsen.
Tissue cultures revealed the presence of Streptococcus contellatus, a bacterium. This happy bug is usually found in the intestines, oral cavity and stomach. However, it can become particularly dangerous when moved to other parts of the body.
However, antibiotics must have kept this microbe from thriving.
Further research revealed that there was an active white blood cell type on the scene, which produces an unusual antibody called IgG4. It's far more than your average antibody. It can reassemble itself in clever ways, turning them into asymmetrical patchworks.
It also has a reputation for causing IgG4-related Disease (RD), an autoimmune condition that can affect any part of the body. This causes inflammation, which in turn whips up pain and misery through highly fibrotic lesions.
The patient was diagnosed with IgG4-related Rhinusitis and given steroids. He was soon back in good health and had clear vision. He was fully recovered three weeks later.
It might make for an episode of House that is half decent, but it also raises an interesting question. Could it have been the patient's SARS-CoV-2 infection? Or were there unrelated, but unfortunate events that led to the patient's infection with SARS-CoV-2?
There may be a link. Although the exact cause of IgG4RD is unknown, it is possible that there are a lot of cytotoxic CD4 positive T-cells hanging around IgG4RD lesions.
This scene would be perfect for a crime-show. A CD4+ T cell that is sensitive to SARS-CoV-2 and was found in COVID-19 patients was taken into interrogation.
SARS-CoV-2, as we all know, is a mastermind in causing havoc with our immune system. It is not a big leap to add another crime against immunity to its list.
Nevertheless, even if you take into consideration an older medical case study that suggested a similar link between IgG4RD and COVID-19 it is too early to draw any definitive conclusions.
It can be difficult to distinguish between meaningful connections and rare coincidences when there are so many cases in this pandemic.
This research was published by JAMA Otolaryngology Head & Neck Surgery.