One of the most crucial questions about an emerging infectious disease such as the new coronavirus is how deadly it is. After months of collecting data, scientists are getting closer to an answer.
Researchers use a metric called infection fatality rate (IFR) to calculate how deadly a new disease is. It is the proportion of infected people who will die as a result, including those who don't get tested or show symptoms.
"The IFR is one of the important numbers alongside the herd immunity threshold, and has implications for the scale of an epidemic and how seriously we should take a new disease," says Robert Verity, an epidemiologist at Imperial College London.
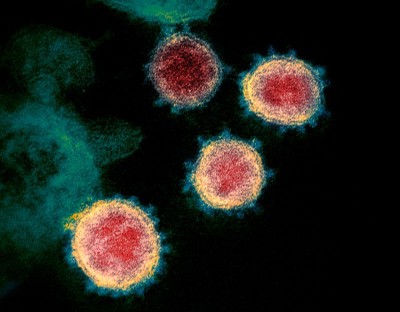
Calculating an accurate IFR is challenging in the midst of any outbreak because it relies on knowing the total number of people infected - not just those who are confirmed through testing. But the fatality rate is especially difficult to pin down for COVID-19, the disease caused by the SARS-CoV-2 virus, says Timothy Russell, a mathematical epidemiologist at the London School of Hygiene and Tropical Medicine. That's partly because there are many people with mild or no symptoms, whose infection has gone undetected, and also because the time between infection and death can be as long as two months. Many countries are also struggling to count all their virus-related deaths, he says. Death records suggest that some of those are being missed in official counts.
Data from early in the pandemic overestimated how deadly the virus was, and then later analyses underestimated its lethality. Now, numerous studies - using a range of methods - estimate that in many countries some 5 to 10 people will die for every 1,000 people with COVID-19. "The studies I have any faith in are tending to converge around 0.5-1%," says Russell.
But some researchers say that convergence between studies could just be coincidence. For a true understanding of how deadly the virus is, scientists need to know how readily it kills different groups of people. The risk of dying from COVID-19 can vary considerably depending on age, ethnicity, access to healthcare, socioeconomic status and underlying health conditions. More high-quality surveys of different groups are needed, these researchers say.
IFR is also specific to a population and changes over time as doctors get better at treating the disease, which can further complicate efforts to pin it down.
Getting the number right is important because it helps governments and individuals to determine appropriate responses. "Calculate too low an IFR, and a community could underreact, and be underprepared. Too high, and the overreaction could be at best expensive, and at worst [could] also add harms from the overuse of interventions like lockdowns," says Hilda Bastian, who studies evidence-based medicine, and is a PhD candidate at Bond University in the Gold Coast, Australia.
Some of the first indications of the virus's deadliness were gleaned from the total number of confirmed cases in China. In late February, the World Health Organization crudely estimated that 38 people had died for every 1,000 with confirmed COVID-19 diagnoses. The death rate among these people - known as the case fatality rate (CFR) - reached as high as 58 out of 1,000 in Wuhan, the city where the virus emerged. But such estimates exaggerated the disease's deadliness because they did not account for the many people who had the virus but were not tested, obscuring the outbreak's true spread.
Researchers tried to address this gap by estimating the IFR from models that projected the virus's spread. The result from these early analyses hovered around 0.9% - 9 deaths for every 1,000 people infected - with a broader range of 0.4-3.6%, says Verity. His own modelling estimated an overall IFR for China of 7 deaths for every 1,000 people infected, increasing to 33 per thousand among those aged 60 or older.
Russell's team also used data gathered from a large COVID-19 outbreak on the Diamond Princess cruise ship in early February to estimate an IFR in China. Almost all of the 3,711 passengers and crew were tested, enabling researchers to count the total number of infections, including asymptomatic ones, and deaths in a known population. From this, his team estimated an IFR of 0.6%, or 6 deaths for every 1,000 infected people.
"The intention of these studies was to gain some ball-park estimates of how deadly COVID-19 is," says Verity.
But researchers also had to make complicated estimates, which still need to be verified, about the number of confirmed cases and the actual number of infected people. "There is value to obtaining rapid early estimates of the IFR, [but] these should be updated as a matter of urgency once better data becomes available," he says.
Widespread population surveys that test people for antibodies to the virus, known as seroprevalence surveys, were expected to help refine IFR estimates even further. About 120 seroprevalence surveys are under way worldwide.

But results from the first antibody studies only muddied the water, suggesting that the virus was less deadly than previously thought. "It got a bit messy," says Russell.
One of the earliest studies tested 919 people in the German town of Gangelt, where a large outbreak had occurred. Of these people, about 15.5% had antibodies against the virus - five times higher than the percentage of people known to have had COVID-19 in the town at the time. The figure was used to estimate an IFR of 0.28%. But researchers noted that the study was based on a relatively small number of people.
Other early seroprevalence studies did not properly account for the lack of sensitivity and specificity in the antibody test kits that were used, or for discrepancies between the sampled and underlying populations, says Verity.
These issues could have inflated estimates of the total number of infected people and so made the virus seem less deadly, he says. Equally, if COVID-19 deaths go undetected - a problem in many countries that aren't testing all deceased people for the virus - that, too, can bias the fatality rate, says Gideon Meyerowitz-Katz, an epidemiologist and PhD candidate at the University of Wollongong, Australia.
Some larger seroprevalence studies have emerged in recent weeks, and these estimate a higher fatality rate than do early studies. One survey, posted on medRxiv, of more than 25,000 people across Brazil, estimated an IFR of 1%.
Another survey that tested more than 60,000 people across Spain reports a prevalence of 5%, although the results have not been formally analysed. The survey team did not calculate a fatality rate themselves, but on the basis of the results, Verity estimates that Spain has an IFR of around 1% - or 10 deaths for every 1,000 infected individuals.
Several researchers, including Russell and Verity, find it interesting that a growing number of studies from different regions have estimated IFRs in the range of 0.5-1%. But other scientists are cautious about suggestions of agreement. "The trend is potentially more luck than anything else," says Meyerowitz-Katz.
Marm Kilpatrick, an infectious disease researcher at the University of California, Santa Cruz, also notes that most of the serological data haven't been published in scientific manuscripts. It's hard to know when and how they were collected, and to properly calculate an IFR that accounts for the delay between people getting infected and dying, he says.
Kilpatrick and others say they are eagerly awaiting large studies that estimate fatality rates across age groups and among those with pre-existing health conditions, which will provide the most accurate picture of how deadly the disease is. One of the first studies to account for the effect of age was posted on a preprint server last week. The study, based on seroprevalence data from Geneva, Switzerland, estimates an IFR of 0.6% for the total population, and an IFR of 5.6% for people aged 65 and older.
The results have not been peer reviewed, but Kilpatrick says the study addresses many of the issues in previous seroprevalence surveys. "This study is fantastic. It's precisely what should be done with all of the serological data," he says.