The Seattle research team that first uncovered COVID-19 spreading in US communities has been asked to stop testing for the disease. The decision by the US Food and Drug Administration (FDA) to prevent the SCAN project from analysing nose swabs sent from people's homes-and reporting the results- is likely to be temporary. But it deflates local and national public-health initiatives.
"SCAN provided valuable data to help us more completely understand the epidemiology of the outbreak," says Jeff Duchin, a health officer at the public-health department for Seattle and King County in Washington state. The programme processed 20,000 tests during the past 10 weeks and helped to reveal which communities in Seattle were being hit hardest by COVID-19. Duchin says the city has begun to integrate the programme into its contact tracing, so that people who have been exposed to the virus can find out whether they've been infected and might pass it on to others.

The project, which is backed by philanthropist Bill Gates, has already navigated a regulatory thicket and won key approvals from state authorities. The FDA's request to pause testing on 12 May frustrates many researchers developing diagnostics that can be conducted partially or fully outside hospitals. The SCAN group was the first to roll out such tests in the United States and - as importantly - to partner with local health authorities to deploy the diagnostics strategically. As businesses begin to reopen in the United States this month and next, many people argue that the kind of testing that SCAN provided is needed more than ever.
"The Seattle group was literally the only group that has really figured out these logistics, and was trying to scale this, and now you want to shut them down?" asks Sri Kosuri, co-founder of Octant, a biotech start-up in Emeryville, California, that is developing tools to diagnose COVID-19. "It blows my mind," he says.
SCAN - which stands for the Seattle Coronavirus Assessment Network - has its roots in the Seattle Flu Study, in which people around the city swabbed their own noses and sent the samples to a lab at the University of Washington, where researchers analysed them for the presence of influenza viruses. To understand how the flu spreads and hopefully stop it, researchers needed to test people outside hospitals. The same idea holds for the coronavirus. And as COVID-19 was spreading around the world in February, the team retooled its assay to identify the new virus.
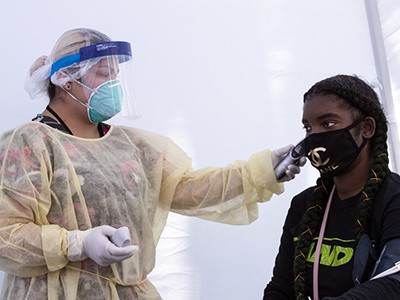
Robin Patel, president of the American Society for Microbiology, who is based at the Mayo Clinic in Rochester, Minnesota , says that researchers have long called for diagnostic tests to be deployed outside of healthcare settings. "This push is being accelerated now by COVID-19, because the reasons to do this are so apparent in an outbreak." A model that requires health workers to draw samples can't easily be scaled up. It's labour intensive, and is risky for the workers required to stick long swabs up people's noses. Moreover, by coming into clinics, people could either pick up an infection or spread one.
In late February, the SCAN team cleared a first set of regulatory hurdles with the US Centers for Disease Control and Prevention. Next, the group analysed about 30 specimens with its own test alongside other assays in clinical labs, to vet its= accuracy. With the data from these experiments, Washington's department of health authorized the researchers to screen people and return the results to them. Seattle's health department discusses SCAN on its official blog. It says the effort helps to show whether social distancing is working, and it slows the spread of the coronavirus because more people know their status and can isolate if necessary. Duchin says: "I have no reason to question the accuracy of the test."
The researchers assumed that they were in the clear because the FDA had granted Washington state the ability to authorize emergency use of COVID-19 tests. In February, FDA guidelines precluded at-home testing from this type of provision, but made no mention of at-home specimen collection, which is how SCAN operates. As of 11 May, however, updated FDA guidelines do specify that tests with at-home collection need to be assessed by the agency.
On 12 May, Bill Gates posted a blog entry on his personal website, saying that the project was testing 300 people per day, with plans to do more. Later that day, the FDA asked SCAN to stop testing until it receives agency authorization.
An FDA spokesperson explains that anything that requires a person to take samples themselves, at home, raises concerns. For example, the agency wants to ensure that samples remain stable if they end up spending a long time in a hot vehicle on the way to a lab. Since 21 April, the FDA has green-lit three home-based tests, developed by the companies LabCorp and Everywell and by Rutgers University in New Jersey.
The FDA has requested data from the SCAN team's first 17,000 samples, as well as information about the programme and its experimental results. The group has scrambled to provide this: for example, it reports that RNA from the coronavirus can still be detected in its swabs after incubating for 9 days at 28 °C - suggesting that samples can survive sitting in a truck. While the researchers wait for the FDA to review their data, a spokesperson says, the team is considering alternatives such as restarting the programme under the auspices of a study.
Researchers tend to agree that quality control is required, and they understand that the FDA is struggling to catch up with a flood of applications from dozens of test developers. Still, Fyodor Urnov, a bioengineer at the Innovative Genomics Institute at the University of California, Berkeley, says the need for testing outside hospitals is so urgent that something has to bend.
Homeless shelters, nursing homes and other shared living facilities should screen residents regularly regardless of their symptoms, to stop outbreaks before they explode, he says. Restaurants and other businesses might want to screen their employees when they reopen and, ideally, hundreds of thousands of contacts of infected people would be tested.

"I see no way forward except self-administration of tests," Urnov says. Although the FDA has adjusted its policies to facilitate at-home testing, Urnov worries the process remains too slow. One option, he suggests, is for the FDA to work more closely with public-health departments and scientists, to share data and find out what they need to control the coronavirus.
Kosuri agrees. He argues that a degree of uncertainty should be acceptable when it comes to routine testing of people who aren't in need of clinical care. Tests that many research groups are developing across the United States will have less data to back them than well-established tests. Inevitably, some of these will turn out to be less reliable than expected, but Kosuri says that's okay. "The relevant question is not, 'Is the test as good as one conducted in a hospital by a trained nurse practitioner?'" Kosuri says. "The question is whether it is better than not being tested at all."