There was a lot of documentation about how rangk quackery was being integrated into medicine to create a fusion calledintegrative medicine. The acronym forcomplementary and alternative medicine was thrown away because its adherents didn't want the nostrums that they added to science-based medicine to be described as "alternative" Almost every other topic seemed to be pushed aside as a result of the Pandemic hit. Even though we haven't been paying as much attention to it as we used to, it doesn't mean that it didn't happen during the Pandemic. I was reminded of the continued use of pseudoscience in medicine last week, which led me to write about a four year follow up study of a negative study of acupuncture for joint pain caused by a class of drugs commonly used to treat breast cancer I didn't expect to be reminded of how much quackery is infiltrating cancer and how much the largest professional society in the world supports it. That reminder came in the form of a news story from Healio, Guideline provides recommendations to manage cancer pain and recommends some forms of "integrative medicine" to manage cancer pain. The guidelines were part of a project between the ASCO and SIO. The Healio publication popped up in my feed over the weekend because I missed their original online publication. The Healio story was spun in a way that was clear.
The study — the first meta-analysis to examine natural, nonpharmacologic approaches to treat cancer pain — resulted in development of guidelines published in Journal of Clinical Oncology. Healio spoke with researcher Jun Mao, MD, chief of the integrative medicine service at Memorial Sloan Kettering Cancer Center, about the importance of the study and the implications of the findings.
The study was summarized by Dr. Mao. There are more than one recommendation in the guidelines, which is why Dr. Mao focused on three of them. He would have been interested in highlighting more plausibleintegrative treatments, such as herbal medicines, which, depending on the specific herbs, may actually contain pharmacologically active components, in particular given that the paper itself states that the panel constructing the guidelines had. I was interested in how little information was given to the second question. There are two things you need to know before I start digging. Dr Mao is a past president of SIO. The Journal of Clinical Oncology is thought to be one of the best journals for cancer research. It is one of the most read and influential journals with an impact factor of 50.717. This is the highest for a journal. The New England Journal of Medicine, a general medical journal, has an IF of 176.079, Nature, 69.504, and Science, 63.714. JCO is in at least the top 20 journals in the world, and it is widely read by every oncologist, radiation oncologists and surgical oncologists. ASCO clearly puts its weight behind guidelines for promotingintegrative cancer in JCO. ASCO has gone all-in with quackery. framing is important when it comes tointegrative medicine orintegrative cancer. It is useful to see how Mao and his team frame the questions to be answered and the evidence that led them to do it. After correctly emphasizing that pain is a common problem in cancer patients and can be due to cancer, cancer treatments, or a combination of the two, Mao et al write.
As pain in patients and survivors of cancer is complex with different etiologies (eg, tumor burden, treatment-related, and non–cancer-related) and varying presentations (eg, neuropathic and musculoskeletal) and duration (eg, acute and chronic), pain management requires an interdisciplinary approach and should include both pharmacologic and nonpharmacologic treatments, where appropriate.2
No one would disagree with such a representation of pain management as long as it was not offensive. What is defined as a non-pharmacological treatment? Evidence-based treatments for pain are not the same as CAM orintegrative medicine, no matter how much advocates try to convince you that their nostrums are science- and evidence-based. This is a common framing by the advocates of medicine.
An estimated 40% of patients with cancer use integrative medicine on an annual basis.12-14 The key guiding principle of integrative medicine is to use these interventions along with conventional pain management approaches (eg, medications, radiation, injections, and physical therapies) and it is not intended to replace conventional interventions.9 Patients often seek integrative medicine because they perceive that conventional medical treatment is not completely meeting their needs, fear side effects from pharmacotherapies, prefer a holistic approach, or because it has been recommended by their family or health care providers.15-18 A growing number of well-conducted randomized controlled trials (RCTs) have found that interventions such as acupuncture or massage can alleviate pain in patients and survivors of cancer.19-21
First, present the unmet medical need in an unobjectionable way that can't really be argued against, if at all, in this case, better pain management in cancer patients. For that unmet need, frameintegrative medicine as non-pharmacological treatment. In order to come up with such large percentages, we need to appeal to the popularity ofintegrative medicine. The data that supposedly shows that placebos work in order to justify your study will be positive. How did these guidelines come to be? An expert panel was convened to develop clinical practice guideline recommendations on the basis of a systematic review of the health literature, which was done thusly.
This SR-based guideline product was developed by an international multidisciplinary Expert Panel, which included a patient representative and a health research methodologist (Appendix Table A2, online only). The Expert Panel met via video conferences and corresponded through e-mail. Based upon the consideration of the evidence, the authors were asked to contribute to the development of the guideline, provide critical review, and finalize the guideline recommendations. The guideline recommendations were sent for an open comment period of two weeks allowing the public to review and comment on the recommendations after submitting a confidentiality agreement. These comments were taken into consideration while finalizing the recommendations. Members of the Expert Panel were responsible for reviewing and approving the penultimate version of the guideline, which was then submitted to the Journal of Clinical Oncology (JCO) for editorial review and consideration for publication. All SIO-ASCO guidelines are ultimately reviewed and approved by the Expert Panel, the SIO Clinical Practice Guidelines Committee, and the ASCO Evidence Based Medicine Committee before publication. All funding for the administration of the project was provided by SIO.
The authors of these guidelines are all believers. There are many familiar names on the author list. Heather Greenlee is a past president of SIO and she is an author on the study of acupuncture for artificial intelligence-caused joint pain. She has been involved in promoting "integrating" magic into Oncology for all cancer patients as well as being associated with a number of efforts to "integrate" quackery with Oncology. The other person came to mind as well. She is the director of the Institute Institute for Complementary and Integrated Medicine. Mark said back in 2010 that she was a believer in homeopathy. Dr. Witt was the lead author on a desperate attempt to defineintegrative oncology, as he argued that CAM is cost effective without actually showing that it is effective. There is a past president of SIO who believes in acupuncture. I like to look at the strongest recommendation that the panel comes up with, examine the evidence used for it, and then decide if it's justified. There is one recommendation that is the strongest for this set of guidelines, and that is that acupuncture should be offered to patients with arthritis.
Recommendation 1.1.
Acupuncture should be offered to patients experiencing AI-related joint pain in breast cancer (Type: Evidence based, benefits outweigh harms; Evidence quality: Intermediate; Strength of recommendation: Moderate).
“Integrating” magical quackery with medicine
Review of literature.
Four SRs and five RCTs were conducted in the area of acupuncture and AI-related joint and muscle pain.19,27-30,44-47 The most definitive evidence is from a phase III sham-controlled RCT conducted among 226 patients with moderate to severe AI-related joint pain.19 After 6 weeks, true acupuncture reduced pain significantly more than sham acupuncture and standard of care (waitlist control; 2.05, 1.07, and 0.99 points, respectively, on a 0-10 point NRS). After 6 weeks, there were more responders who had a clinically meaningful change in pain (a two-point reduction on a 0-10 scale) 253 in the true acupuncture group compared with the sham and waitlist control groups (58%, 33%, and 31% respectively).
In reference 19 I wrote about the study. It was not a double-blinded study, despite the fact that it included a waitlist. Despite the contortions that the authors went through to justify no blinding of the acupuncturists, the results of the study are very small. I pointed out that the study published this month to examine long-term effects and treatment durability was no more positive than the first one because the differences between the true and sham acupuncture groups fluctuated from nearly zero to still tiny. It was consistent with previous studies of acupuncture use to treat arthralgias that we have written about before, but it was also consistent with placebo effects.
The strongest recommendation in the review was that the evidence quality was intermediate and the strength of recommendation was moderate. It will go downhill quickly from there. The guidelines recommend yoga but the recommendation strength is weak and based on low evidence. With low quality evidence and a weak recommendation, yoga is recommended for people with breast or head and neck cancer.
I think I will just reproduce this chart from the paper, which is rather interesting in and of itself, for reasons that I will list after you have a chance to look at the chart.
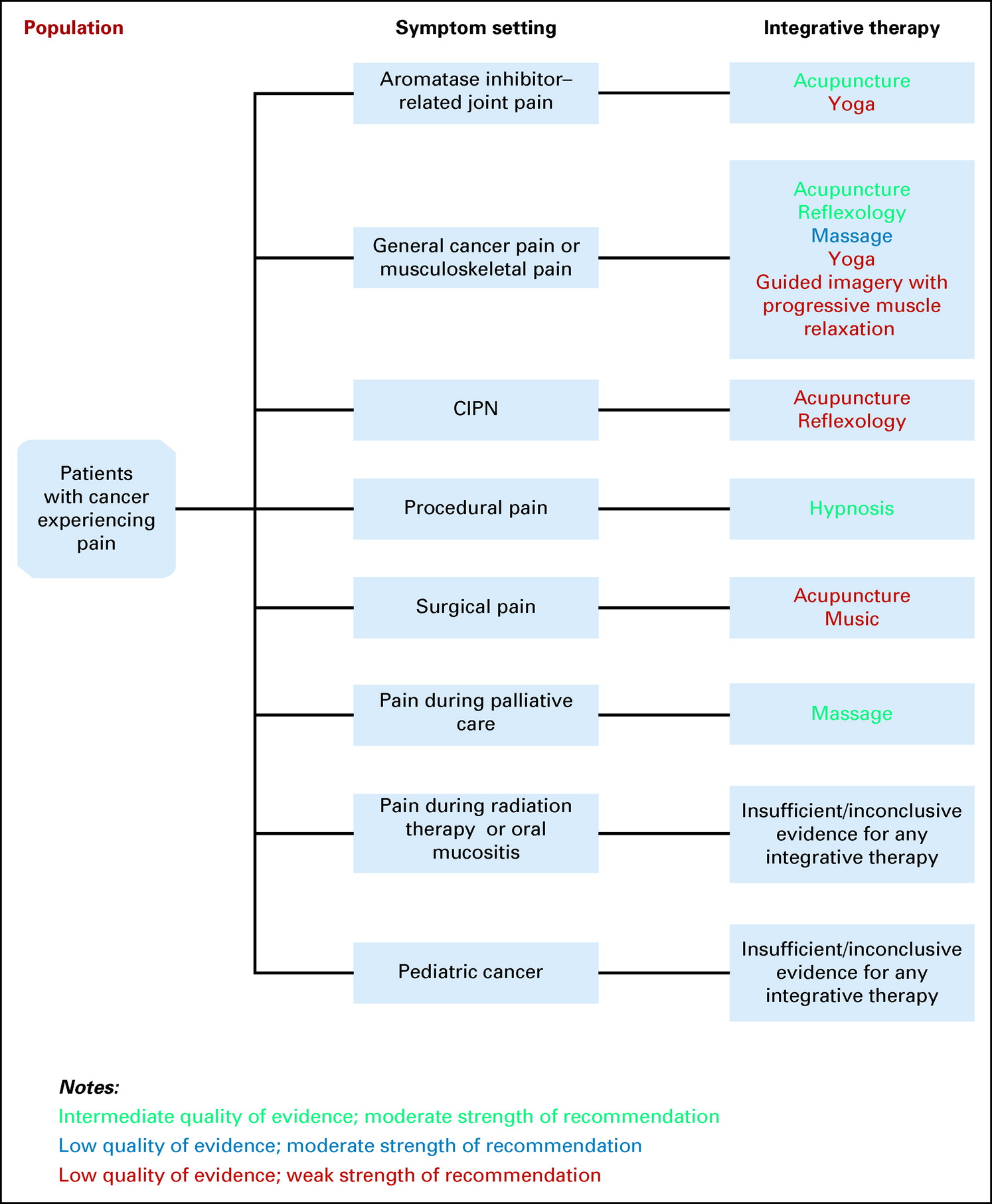
Recommendations forintegrative medicine interventions for pain related to cancer and cancer treatments were made by the SIO-ASCO.
I stole a bit of the thunder by mentioning that the strongest recommendation is moderate, with a caveat that benefits outweigh harms. In any event, notice how little green there is compared to black and blue. The literature search strategy used to search randomized controlled trials, systemic reviews, and meta-analyses should be noted.
The recommendations were developed by using a SR of evidence identified through online searches of PubMed (1990-2021) and Cochrane Library (1990-2021) of RCTs, SRs, and meta-analyses. Articles were selected for inclusion in the SR on the basis of the following criteria:
- Population: Adults and pediatric patients experiencing pain during any stage of their cancer care trajectory
- Interventions: Integrative interventions for pain management, including acupuncture, acupressure, mind-body therapies, and natural products (note: see details in the Data Supplement, online only; therapies focused on pain prevention were not included)
- Comparisons: No intervention, waitlist, usual care (UC) or standard care, guideline-based care, active control, attention control, placebo, or sham interventions
- Outcomes: Pain intensity, reduction, or change in symptoms reported as the primary outcome in published manuscript
- Sample size: Minimum total sample size of 20
Articles were excluded from the SR if they were (1) meeting abstracts not subsequently published in peer-reviewed journals; (2) editorials, commentaries, letters, news articles, case reports, and narrative reviews; or (3) published in a non-English language. The guideline recommendations were crafted, in part, using the Guidelines Into Decision Support methodology and the accompanying BRIDGE-Wiz software program.25 In addition, a guideline implementability review was conducted. On the basis of the implementability review, revisions were made to the draft to clarify recommended actions for clinical practice. Ratings for type and strength of the recommendation, and evidence quality are provided with each recommendation. The quality of the evidence for each outcome was assessed using the Cochrane Risk-of-Bias tool26 by the project methodologist in collaboration with the Expert Panel cochairs and reviewed by the full Expert Panel.
In guideline construction, all of this is standard. I hope that you will be able to glean a bit before I explain, but I will include the flow chart for the literature search and selection for a reason.
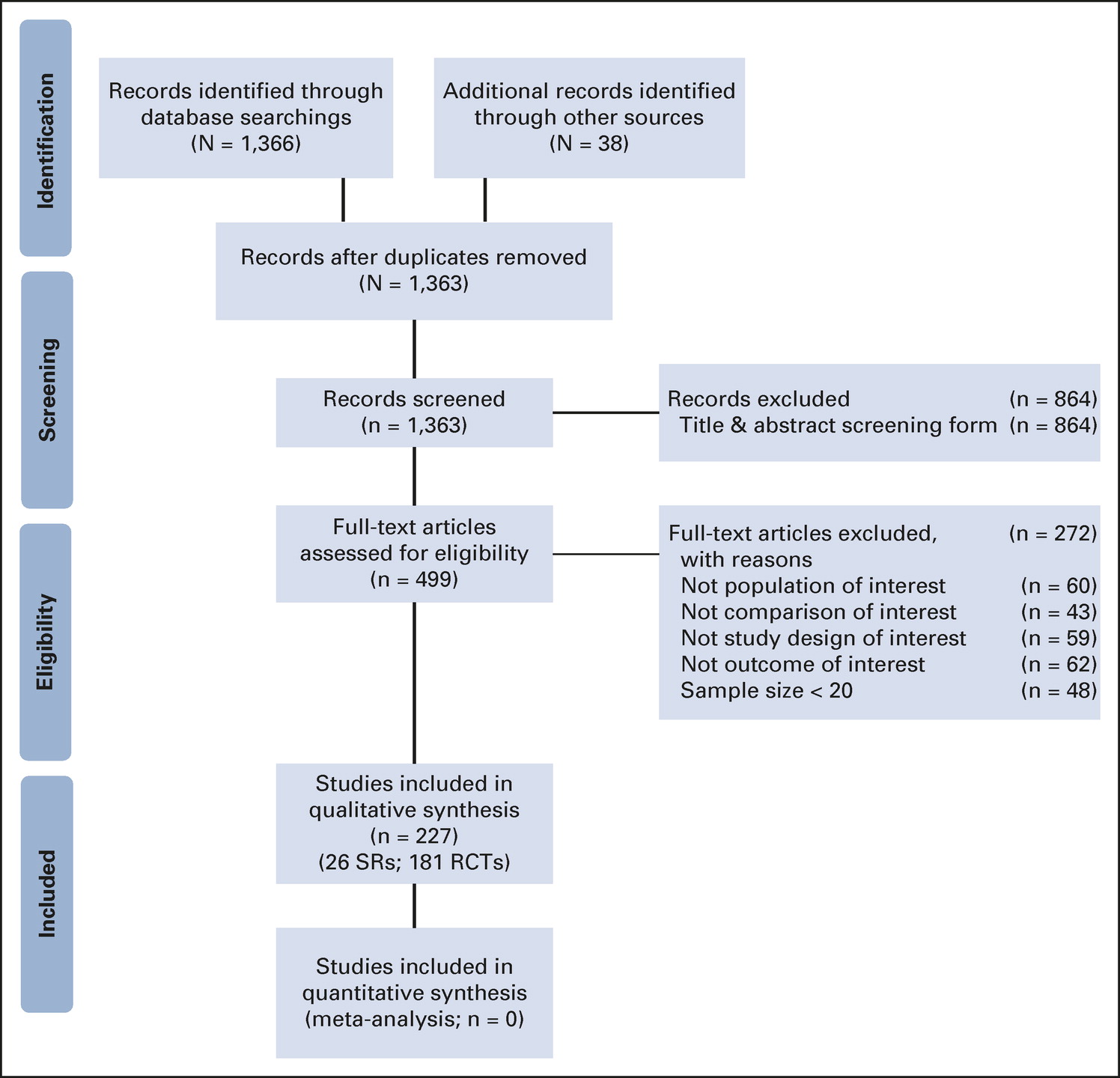
The flow chart shows guidelines.
It is not unusual for the winnowing of articles from initial search to articles used in a systematic review or meta-analysis to be severe, but I was surprised at how few articles were initially involving relatively few therapies.
None of the herbal products made it into the 13 weak to moderate strength recommendations because they were a bust. The evidence for natural products was not conclusive.
There is insufficient evidence to recommend for or against the use of Xiao Zheng Zhitong paste, Jinlongshe granule, Shuangbai San paste, or Xiao-Ai-Tong decoction for general cancer pain. Four trials tested the effects of Chinese herbal preparations on treating general cancer pain, including Xiao Zheng Zhitong paste in patients with a range of different cancer types,207 Jinlongshe granules in patients with gastric cancer,208 Shuangbai San paste in patients with liver cancer,209 and Xiao-Ai-Ton decoction with and without morphine in patients with a range of different cancer types.206 Given that there was only one trial of each treatment intervention, variability in quality of the trials, there are insufficient data to make a clinical recommendation.
It could be either negative or positive.
Two RCTs tested the effects of glutamine on the incidence and severity of peripheral neuropathy.186,187 The first trial was a moderate-size (N = 86) trial comparing oral levo-glutamine compared with no intervention in patients with colorectal cancer receiving oxaliplatin.186 Patients who received levo-glutamine had lower incidence and severity of peripheral neuropathy symptoms; however, the trial did not control for placebo effects. The second smaller trial (N = 43) compared oral glutamate to placebo in women with ovarian cancer receiving paclitaxel.187 There were no differences between groups in incidence of peripheral neuropathy; patients who received glutamate reported lower pain severity. No clinical recommendations can be made on the basis of these results because of low study quality and/or small sample size.
I would have predicted that there would be at least one herbal treatment that showed promise, given that herbal treatments always have the chance of containing one or more pharmacologically active compounds.
We have discussed the biological implausibility of acupuncture a lot. What can one say about the idea that every part of your body is connected to your feet? I found this chart by searching for the term "reflexology".
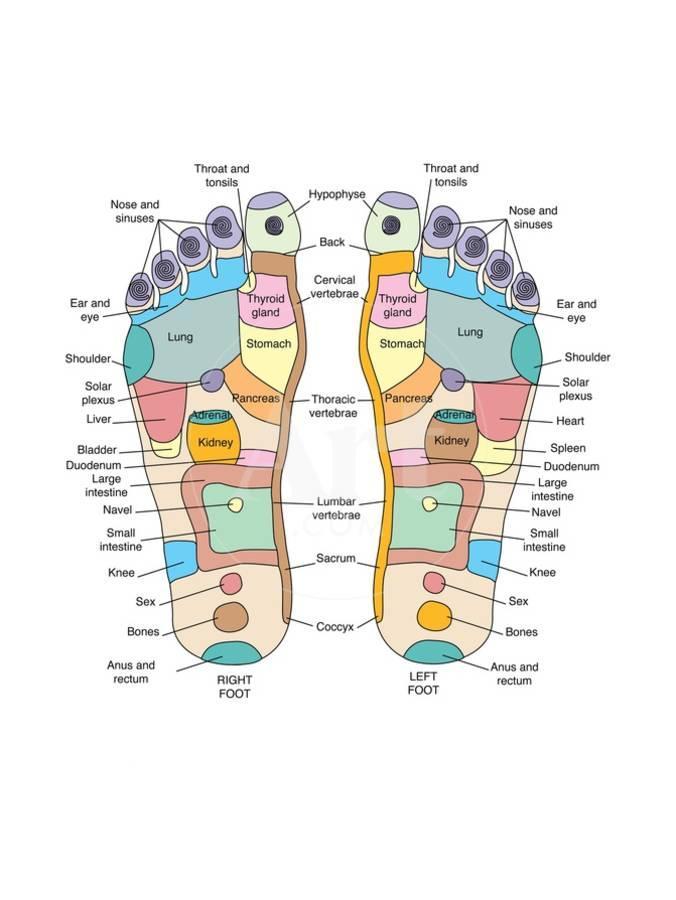
There is a map of feet. This is not how our bodies work.
By applying pressure to certain locations on the foot, you can affect the function of the organ that it maps. Attempts to "modernize" reflexology have failed to make it less ridiculous. Despite its scientific implausibility and lack of evidence, some states still license its practitioners.
I have written many times about how ASCO has embraced the nonsensical pseudoscience behind quackery. Eight years ago, I was appalled by the blatantness of its embrace when I attended an ASCO meeting that featured a major session onintegrative cancer. A few years ago, ASCO endorsed guidelines for the use ofintegrative therapies in the treatment of breast cancer patients, which led to a post by me explaining how harmful this embrace of quackery was to cancer patients. In 2010 JCO published a very disappointing editorial about a cancer treatment that was clearly rank quackery.
ASCO and its journal JCO are not alone, as this sort of integration of quackery with medicine is found in many journals. Despite the inherent contradiction between evidence based andintegrative practices, there are training programs that claim to produce the next generation of evidence based practitioners.
It is hard for me to not see a connection between theTrojan horse that isintegrative medicine and the misinformation that we have been enduring. We have now seen a disturbingly large minority of doctors embrace treatments that are wildly implausible from a basic biology perspective. When you embrace unreality in one area of medicine, how do you prevent it from being metastasized to other areas of medicine? ASCO is usually a champion of science and evidence based medicine. We aren't living in normal times and haven't been since before the Pandemic The embrace of unreality was accelerated by the outbreak of the swine flu.

You can buy an e- book.
Dr. Hall is teaching a video course.
The text is powered by the internet.
 English
English