335 people will die from Covid in the U.S. today, due to the fact that there are highly effective vaccines, treatments and precautions available. Why are people still dying?
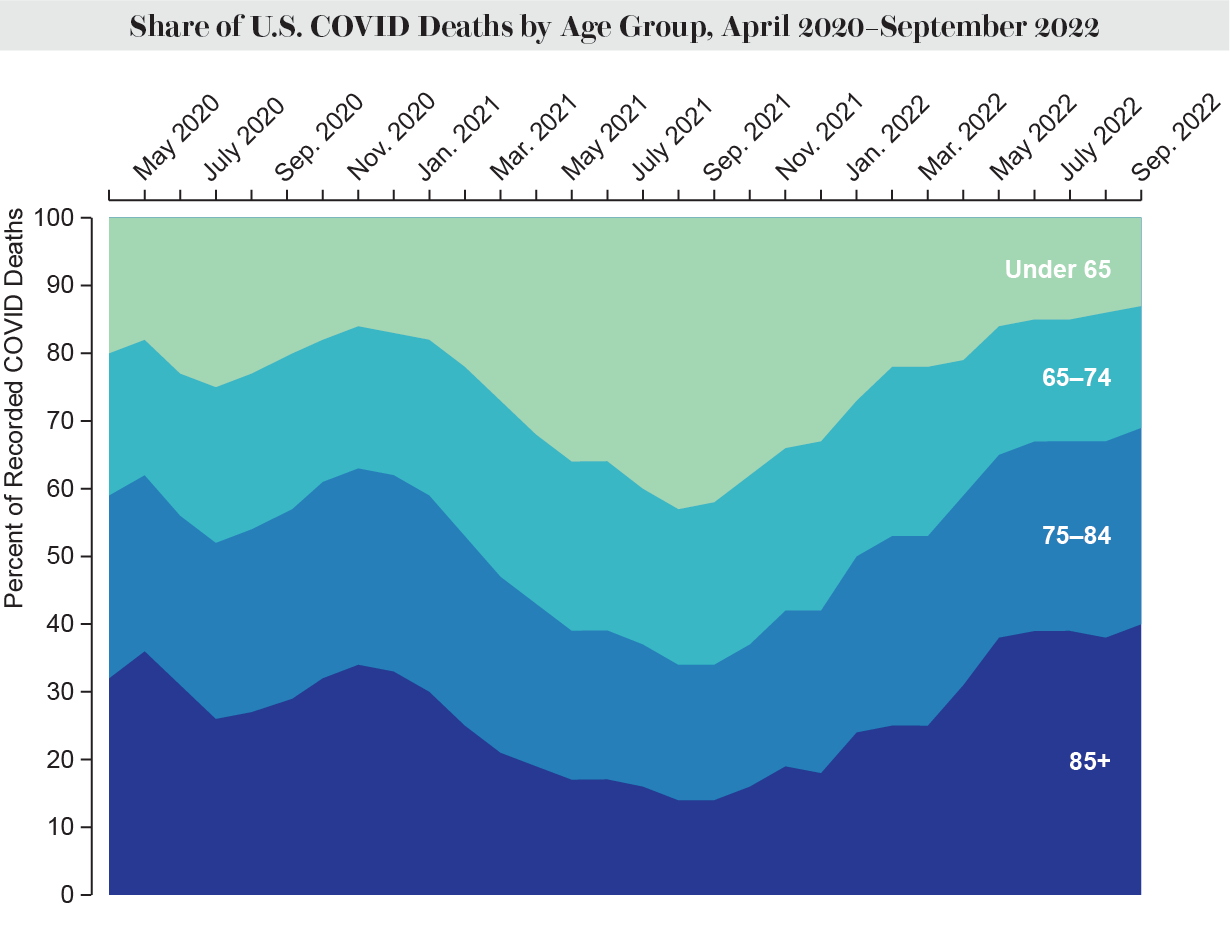
Older people are more likely to die in the Pandemic than before. The burden of mortality is shifting more to people older than 64 as the total number of deaths has fallen. One of the top causes of death for all ages is nursing home deaths. According to a recent analysis by the Kaiser Family Foundation, deaths among people 65 and older more than doubled between April and July. More than a quarter of all COVID deaths were among those over the age of 85, but that share has gone up to at least 38 percent since May.
People's risk levels are affected by where they live. Mortality rose in rural areas by the summer of 2020 despite the fact that the Pandemic first hit urban areas hard. People living in rural areas are dying at a higher rate than people living in urban areas. At the end of September, the rural death rate was 92.2 percent higher than the urban one.
COVID deaths are more likely to be caused by racism and discrimination. The age-adjusted death rates based on race have recently become smaller, but experts predict that will not last.
According to the U.S. Centers for Disease Control and Prevention, the death rate from chronic bronchitis in the U.S. has remained constant for the past several weeks. The United States has the highest number of confirmed COVID deaths of any country. According to the CDC, there have been over one million excess deaths in the US since February 2020. The leading cause of death during the Pandemic was the viral illness. Since the beginning of the crisis, life expectancy in the U.S. has dropped. The co-founder of Marked by COVID, an advocacy network memorializing the victims of the illness, says that it's the first of its kind. I don't believe that will stop soon.
More than 200,000 people have died as a result of COVID in the U.S., and President Joe Biden is bracing for tens of thousands more deaths this winter. About 50,000 deaths are brought about by a bad flu season.
Public funding has waned for the very vaccines and treatments that have lowered the risk of death. The key tools will only be available to those who can afford them on the private market as federal subsidies dry up. If things don't come back, it's scary to think about what will happen.
At the peak of the most recent surge of fatalities in August, 91.9 percent of all deaths were among people 65 and older, the biggest share of any surge in the epidemic.
During the Pandemic, long-term care facilities were hit hard, with residents and staff accounting for one fifth of all deaths. These blows were lessened by vaccinations and treatments. Deaths in nursing homes have gone up again. This number more than doubled from April to August.
Even though most COVID deaths are among the elderly, younger people are dying at higher rates than usual because of the illness. According to a visiting scientist at the Harvard Franois-Xavier Bagnoud Center for Health and Human Rights, young people rarely die in the U.S. Excess mortality for all age groups is high in the U.S., compared to other wealthy countries.
Other patterns are also emerging when it comes to race and ethnicity. Experts say that the changes are likely to be short-lived.
You can sign up for Scientific American's newsletters.
The mortality rates among white people have been close to those among black people. When the total COVID death rate goes up, the deaths of minorities have gone up again. The same pattern of inequity is expected. When the total death counts are lower, white people are dying at a higher rate. Black people die at a higher rate when death counts are higher. American Indians, Alaska Natives and Pacific Islanders, who have had the highest death rates this entire time, are not even acknowledged.
According to a study published in September, deaths from all causes were higher for Indigenous peoples and Pacific Islanders in the first two years of the Pandemic. People of color have been hit harder by the changes. According to a preprint paper that has not yet been peer-reviewed, black, Hispanic and Indigenous people in rural areas had the most deaths from COVID in the U.S. Rural areas with poor access to health care and an older and sicker population are more likely to have these differences.
Vaccinations have helped reduce some differences. The vaccine shrinks racial inequality. It's that easy. Many people of color are put at risk by the same factors. Death rates in communities of color have been higher due to inequitable access.
Being unvaccinated is still a risk factor for death. According to the CDC, unvaccinated people died at six times the rate of those who got the vaccine. Older people who are unvaccinated are 12 times more likely to die than younger people who are vaccine free.
The majority of deaths in the U.S. are now among people who have received a vaccine. In July, 59 percent of COVID deaths were among the vaccine recipients. The vaccines are still highly effective at reducing the risk of death and severe illness, even though they are no longer working. Boosters need to be combined with other precautions in order to prevent illness and death. According to the CDC, people 50 and older who had just one booster were three times more likely to die than people with two or more.
Only a small percentage of Americans over the age of five have received the bivalent booster, which is highly effective against the Omicron variant of the virus. More than 14 million Americans 65 or older have received the updated jab, a higher rate than younger Americans but nothing like the initial two doses. Wrigley- Field says that they have never had the same kind of efforts to make boosters available. Boosters are important to reduce hospitalization and death for everyone but also to weaken chains of transmission and help protect the most vulnerable.
Antiviral drugs can be very effective at preventing hospitalization and death, but they are underused and distributed in a way that is not optimal. A study by the CDC found that zip codes with the most vulnerable people have the lowest levels of antiviral use. A CDC study shows that people of color are less likely than white people to get an immune response. Only 11 percent of people who tested positive for COVID were prescribed drugs. Those with higher incomes received Paxlovid at a higher rate than those with lower incomes. According to an analysis from a medication-dispensing site, 42 percent of U.S. counties were paxlovid deserts.
More than 8 million Americans are at risk of dying from chronic bronchitis. According to the CDC, only a small percentage of them have received Evusheld, a treatment that can prevent severe outcomes for six months at a time.
The crisis is in the middle of it. The most vulnerable will be sentenced to death.
This could be a story about numbers. The thing is not. The story is about people. Faces of Covid is an online project that shows the stories behind the statistics and is intended to honor the lives lost and those who grieve them. When a loved one dies, all of us lose something. If we don't learn the lessons of the Pandemic, we will be hit 10 times harder by the next one, he says. We are proving ourselves to be completely unable to wrap our arms around those kinds of challenges. That makes me fear for the future.