I'm not able to do what I used to.
Many of the patients that we treat for lung disease tell us this even months after their initial diagnosis. They have yet to return to their pre-COVID-19 baseline, struggling with activities ranging from strenuous exercise to doing laundry, even though they have survived the most life threatening phase of their illness.
As many as one in five Americans have been affected by long COVID.
Brain fog, fatigue, cough, and shortness of breath are some of the symptoms of long cobra.
Understanding the causes of long COVID is a focus of the Biden-Harris administration.
Some breathing problems are not related to the lungs.
Looking at the lungs' basic functions and how they can be affected by disease can help clarify what is on the horizon for some patients.
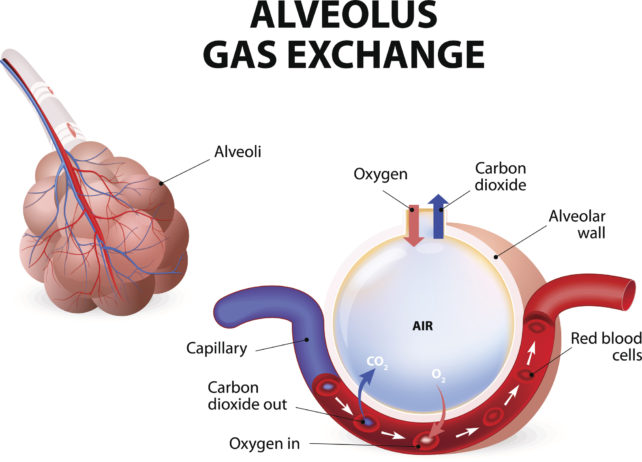
The lungs bring oxygen-rich air into the body and excrete carbon dioxide. When air enters the lungs, it is brought into close proximity with the blood, where it diffuses into the body.
This process requires an extraordinary coordination of air flow and blood flow.
All the way out to the little balloons at the end of the airway are in close contact with your blood vessels.
By the time a molecule of oxygen gets down to the end of the airway, there are about 300 million of these little alveoli, with a total surface area of over 1000 square feet.
Lung function can be affected by damage to the airway, which can lead to difficulties in breathing.
There is obstruction of air in and out of the lungs.
There are two common causes of impairments.
Damage from smoking is one of the main causes of narrowed airways in these diseases. Patients experience difficulties blowing air out of their lungs.
Some patients who have recovered from COVID-19 have continued obstruction of their air flow.
This condition is usually treated with inhalers that deliver medication that opens up the airway. Recovering from COVID-19 may be helped by such treatments.
restriction is a type of lung disease that is difficult to expand. The amount of air they can take in is reduced by restriction.
The formation of scar tissue in the lungs is a result of restriction.
Gas exchange with the blood is more difficult due to the thick walls of the alveoli.
This type of scarring can occur in chronic lung diseases, such as IpF, or as a result of severe lung damage in a condition called ARDS.
There are injuries in the lungs that can cause ARDS. 25 percent of patients who recover from ARDS go on to develop lung diseases.
Patients who have recovered from COVID-19 are more likely to develop restrictive lung disease, according to researchers.
Recovery rates for patients who need a ventilator are similar to those for patients without one. The long-term recovery of lung function in these patients is not known. Clinical trials are taking place for drugs that treat fibrotic lung disease.
If blood flow to the alveoli is disrupted, the lungs can't complete their function.
There is an increased risk for blood clot with Covid-19. Blood clot travel to the lungs can cause a life threatening pulmonary embolism.
Blood clot can cause chronic problems with blood flow to the lungs, a condition known as chronic thromboembolic pulmonary hypertension.
A small percentage of patients who develop a pulmonary embolism for reasons other than COVID-19 go on to develop a chronic problem.
The blood vessels of the lung can be damaged by severe COVID-19 infections.
Lungs can work less well in three general ways. There are still ways to treat long-term lung damage.
It's important for clinicians to follow up with patients who have recovered from COVID-19 if they have persistent symptoms.
Rates of long COVID are associated with severe cases of COVID. There are a number of risk factors for the development of long COVID.
The underlying mechanisms of how different types of lung-related conditions that result from COVID-19 infection are studied by researchers.
Researchers would be able to develop targeted treatments that would speed recovery and make patients feel better once again.
Everyone can use preventive measures, such as good hand hygiene and masking, when appropriate.
Jeffrey M. Sturek is an assistant professor of medicine at the University of Virginia.
Under a Creative Commons license, this article is re-posted. The original article is worth a read.