Medical technology that physicians often take for granted is pulse oximeters. pulse oximeters were used to monitor the oxygen content of a patient's blood with a clip placed on a finger or ear. The severity of the pneumonia caused by COVID-19 is determined by the amount of oxygen in the air. The saturation of the red blood cells is an indicator of the severity of the disease. Silent hypoxic, also known as happy hypoxic, is a phenomenon in which patients are hypoxic without any of the normal symptoms. Stories of patients with dangerously low oxygen saturations scrolling on their phones, chatting with doctors, and generally describing themselves as comfortable quickly became a staple among doctors treating the new coronaviruses disease.
Monitoring patients during surgery or with any disease that can affect the function of their lungs and hearts can be done with pulse oximeters. They are used to monitor patients undergoing general anesthesia, as well as patients in other healthcare settings. If pulse oximeters weren't so accurate for a large group of people, what would that mean? As I was driving to work last week, I listened to an NPR report about studies showing that pulse oximeters don't always give accurate estimates of oxygen saturation in patients with darker skin.
Over the past two years, the pulse oximeter has become a crucial tool for tracking the health of COVID-19 patients.
The small device clips onto a finger and measures the amount of oxygen in a patient’s blood. But a growing body of evidence shows the device can be inaccurate when measuring oxygen levels in people with dark skin tones.
A study published on Monday only adds to this concern.
Researchers analyzing pre-pandemic health data also find those measurements resulted in patients of color receiving less supplemental oxygen than white patients did.
“We were fooled by the pulse oximeter,” says the study’s lead author Dr. Leo Anthony Celi, who’s clinical research director and principal research scientist at the MIT Laboratory of Computational Physiology.
“We were given the false impression that the patients were okay. And what we showed in this study is that we were giving them less oxygen than they needed,” he says.
An anecdote about a doctor who gave a false impression to a patient with COVID-19 was included in the story.
Looby-Gordon, who’s a physician at Boston Medical Center, found herself on the phone with a triage nurse at a Florida hospital, arguing that her own son — who was very sick with COVID-19 — needed to be admitted to the hospital.
“‘Well, yeah, he is looking pretty short of breath,'” Looby-Gordon remembers the nurse responding, “‘but his oxygen levels are good.'”
The nurse was basing this on the reading from the pulse oximeter clipped to his finger, but this assessment did not feel right to Looby-Gordon.
She got off the phone with the nurse and spoke with other doctors at her medical center. One of them reminded her of a 2020 article in the New England Journal of Medicine showing the pulse oximeter tends to be inaccurate in people with dark skin tones.
“On top of that, my son is — this sounds strange — but very dark, very dark complexion,” says Looby-Gordon.
Sure enough, later when her son was given a more invasive test for measuring blood oxygen, it showed his oxygen levels were actually dangerously low.
It was most likely a blood draw to measure the oxygen level in the patient's arteries. Many physicians are unaware of the issue with pulse oximetry. According to the NPR story, Dr. Looby-Gordon had to argue with doctors that her son was sicker than his home pulse oximeter readings suggested, because she didn't know how the device could be so misleading.
This phenomenon is not new. COVID-19 brought about a greater understanding of racial disparity in medical care and how science-based medicine needs to pay more attention to them.
Sampling blood and measuring blood gases are the most accurate ways to determine oxygen saturation. The measurement is referred to as SaO2 as opposed to the saturation measurement obtained by pulse oximetry. The partial pressures of oxygen and carbon dioxide in the blood are provided by the Abg. It is possible for doctors to determine if there is enough oxygen in the blood and if there is enough acid in it. Monitoring ABGs requires either an in-arterial catheter from which blood can be drawn or a stick to draw blood. Although only estimating SpO2 and pulse rate, a pulse oximeter can take continuous readings.
The light absorbances of hemoglobin can be different when it doesn't have oxygen bound to it. In brief, pulse oximeters use a pair of LEDs, one of which emits red light and the other of which emits IR, taking advantage of the difference in absorption of that light between deoxygenated hemoglobin and oxygenated hemoglobin.
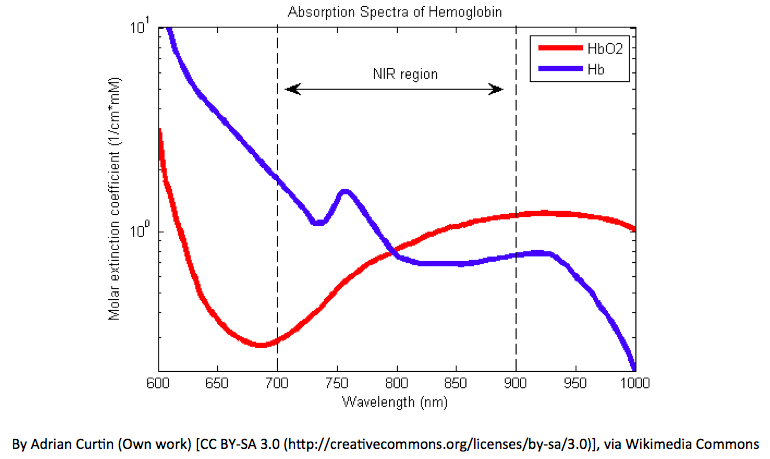
The absorption spectrum is related to pulse oximetry.
Hb allows more red light to pass through, while Hb allows more IR light to pass through. The device works from here.
- The LEDs sequence through their cycle of one on, then the other, then both off about thirty times per second.
- The amount of light that is transmitted (in other words, that is not absorbed) is measured.
- These signals fluctuate in time because the amount of arterial blood that is present increases (literally pulses) with each heartbeat.
- By subtracting the minimum transmitted light from the peak transmitted light in each wavelength, the effects of other tissues is corrected for allowing for measurement of only the arterial blood.
- The ratio of the red light measurement to the infrared light measurement is then calculated by the processor (which represents the ratio of oxygenated hemoglobin to deoxygenated hemoglobin).
- This ratio is then converted to SpO2 by the processor via a lookup table based on the Beer–Lambert law.
This causes the pulse oximeter to produce waveforms that look similar to this.
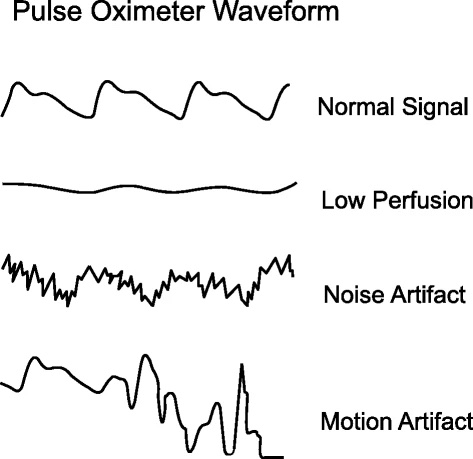
The pulse oximetry is used to measure blood pressure.
It has been known for a long time that nailpolish can affect pulse oximetry readings. It was a surprise. The measurement of how much light is absorbed at different wavelength is interfered with by a pigment. There are some interesting potentials failure of pulse oximetry that have been appreciated. In these cases, pulse oximetry readings show a false elevated SpO2. Doctors are taught that pulse oximetry is not accurate estimating SpO2 during training.
The inaccuracy of pulse oximetry in people with more colored skin is an issue that has been known for a long time, but relatively little attention was paid to this issue before the outbreak. The reliability of smart watches and fitness monitors was negatively impacted by issues that negatively impacted their reliability after they added a pulse oximeter. This Washington Post story is related.
The tiny type at the bottom of Apple’s website says its blood oxygen app is “not intended for medical use” and is “only designed for general fitness and wellness purposes.” Fitbit’s small print says its blood-oxygen app is “not intended to diagnose or treat any medical condition” and is useful to “help you manage your well-being and keep track of your information.”
The reporter noted.
Over several days of comparing my second Apple Watch’s measurements to my FDA-approved finger oximeter, Apple’s readings most often differ by two or three percentage points — though they’ve also sometimes exactly matched, and sometimes have been as much as seven percentage points lower.
It's oddly enough.
When I tested the Apple Watch on a colleague whose skin is darker than mine, the results were also off from the finger pulse oximeter, but less wildly so.
The Apple watch has been found to produce accurate SpO2 readings.
The pulse oximeter feature on the Apple Watch was turned off because it was chewing up the battery and reporting low oxygen saturation readings that were not accurate.
The first study that looked at pulse oximetry in non-white patients was published in 2020. The University of Michigan gave me the data for the study, which looked at 10,789 pairs of measures of oxygen saturation by pulse oximetry and arterial oxygen saturation in blood gas obtained from 1,333 white and black patients.
The study concluded.
In unadjusted analyses, the area under the receiver-operating-characteristic curve for detecting an arterial blood gas oxygen saturation of less than 88% according to the oxygen saturation on pulse oximetry was 0.84 (95% CI, 0.81 to 0.87) among Black patients and 0.89 (95% CI, 0.87 to 0.91) among White patients (P=0.003). In the multicenter cohort, the unadjusted analyses involving patients with an oxygen saturation of 92 to 96% on pulse oximetry showed an arterial blood gas oxygen saturation of less than 88% in 160 of 939 measurements in Black patients (17.0%; 95% CI, 12.2 to 23.3) and in 546 of 8795 measurements in White patients (6.2%; 95% CI, 5.4 to 7.1).
Thus, in two large cohorts, Black patients had nearly three times the frequency of occult hypoxemia that was not detected by pulse oximetry as White patients. Given the widespread use of pulse oximetry for medical decision making, these findings have some major implications, especially during the current coronavirus disease 2019 (Covid-19) pandemic. Our results suggest that reliance on pulse oximetry to triage patients and adjust supplemental oxygen levels may place Black patients at increased risk for hypoxemia. It is important to note that not all Black patients who had a pulse oximetry value of 92 to 96% had occult hypoxemia. However, the variation in risk according to race necessitates the integration of pulse oximetry with other clinical and patient-reported data.
One in six black patients in the multicenter cohort with an SpO2 between 92- 98% actually have hypoxemia, compared to one in 16 white patients.
A study about a group of patients in the intensive care unit was published in the Journal of the American Medical Association. The retrospective cohort study was based on the medical information mart for intensive care. The data from 40,000 patients who were admitted to the intensive care units at the Beth Israel Deaconess Medical Center is included in this dataset. The database is only up-to-date through the year, so it did not include COVID-19 patients.
Patients who were documented with a race and ethnicity as Asian, Black, Hispanic, or White were admitted to the intensive care unit for at least 12 hours before needing respiratory support. Oxygenation levels and flow rates for up to 5 days from the time of intubation were analyzed. The primary outcome of this case was time-weighted average supplemental oxygen rate, with co-variates including race and ethnicity, sex and SpO2–hemoglobin oxygen saturation discrepancy. Vasopressors cause blood vessels to relax and expand, while inotropes make the heart pump harder.
The overestimation of SpO2 in darker skinned patients results in a lower oxygen use. This lower oxygen use for a given level of unsuspected hypoxemia likely results in poorer outcomes as well, as suggested by a study from 2021, that examined five databases with data from nearly 88,000 patients total.
Patients who are critically ill may be the only ones who have this disparity. Two weeks ago, the Veterans Administration published a study that looked at patients in general care in VA hospitals.
In general care inpatient settings across the Veterans Health Administration where paired readings of arterial blood gas (SaO2) and pulse oximetry (SpO2) were obtained, black patients had higher odds than white patients of having occult hypoxemia noted on arterial blood gas but not detected by pulse oximetry. This difference could limit access to supplemental oxygen and other more intensive support and treatments for black patients.
The authors are done.
Errors in pulse oximeters could be due to a combination of systematic error or bias, which is reproducible across measurements, as well as random error or noise.30 Because pulse oximeter error is due to a combination of both processes, the magnitude of pulse oximeter error might not be the same each time a reading is taken. We empirically show that these errors could result in clinically meaningful differences in the interpretation of pulse oximetry across racial groups. In patients with two pairs of SpO2-SaO2 readings measured on the same day, a well aligned SpO2-SaO2 pair for white patients was associated with low levels of occult hypoxemia on subsequent pairs; such concordance might be reassuring in many clinical scenarios. This concordance was less true for black patients, and these differences should be considered in deciding whether to obtain an arterial blood gas reading in appropriate clinical situations until non-racially biased pulse oximeters are in use.
The study found a small difference in the rate of hypoxemia between white and black patients, but it was still significant and could be due to the patient population under study being less ill than in the other studies. The trend is getting more clear because of the variability in results examining the accuracy of pulse oximetry. There is a growing body of evidence that shows that pulse oximeters can be dangerously inaccurate in some patients with darker skin.
It’s been known for decades that the devices are less accurate in patients with darker skin and those wearing nail polish, but new interest and a stream of research about potential racial bias in the devices has been sparked by the racial disparities seen in Covid deaths and treatment. The measurement of oxygen levels using the devices has played a critical role in determining which Covid patients are admitted to the hospital and given supplemental oxygen and other therapies. The devices, invented in the 1970s, were tested on largely white populations.
“This is telling us what we see as disparities could be due to technology that is not optimized for all populations,” said Leo Anthony Celi, a co-author of the JAMA Internal Medicine paper, and an ICU physician and a principal research scientist at the Institute for Medical Engineering and Science at MIT who helped create the large public database of ICU patients used in the study. “We’re seeing the downstream effect. It performs poorly as soon as you apply it outside the demographic it was designed for.”
The FDA updated its safety communication in June.
The FDA continues to evaluate all available information pertaining to factors that may affect pulse oximeter accuracy and performance. Because of ongoing concerns that these products may be less accurate in individuals with darker skin pigmentations, the FDA is planning to convene a public meeting of the Medical Devices Advisory Committee later this year to discuss the available evidence about the accuracy of pulse oximeters, recommendations for patients and health care providers, the amount and type of data that should be provided by manufacturers to assess pulse oximeter accuracy, and to guide other regulatory actions as needed. Further details concerning the agenda, timing, and location of the Advisory Committee meeting will be announced in the coming weeks.
Clinical trials for the approval of pulse oximeter devices should include at least two darkly-pigmented people, or 15% of the subject pool, whichever is larger according to FDA guidance. It's not clear if this is enough to make sure that device makers fix this problem.
It is becoming harder to deny that there are differences in oximeter accuracy due to race pulse. The response from device manufacturers to the findings has not always been positive. The founder and CEO of Masimo published an editorial after stating that he was co-inventor of the modern day measure-through motion and pulse oximetry. He asked if the differences were due to the differences between black and white populations, and if the difference was caused by the differences between black and white populations. He wondered if tissue damage and poor circulation, which afflicts Black people more than any other group, had affected the pulse oximetry readings. He asked if there was a correlation between the percentage of patients with methemoglobinemia and the drugs used to treat it.
Hydroxychloroquine, the anti-malarial drug that was used for COVID-19, was blamed for not working.
One of them, hydroxychloroquine, which has been recently used on COVID-19 patients, has been shown to dramatically elevate MetHb in Black patients. MetHb not only causes huge errors in pulse oximetry, including biasing pulse oximetry readings, but also can kill the patient if it’s not detected and treated immediately. Did the Michigan study account for this?
He became angry at the end.
What these publications did is regretful:
- With very little explanation and underlying data, the Michigan authors sent in their findings.
- The New England Journal of Medicine published their findings seemingly without asking for the kind of data that you’d expect in a scientific journal.
- The Boston Review and the New York Times rushed to give the purported bias in a pulse oximeter a racist narrative.
We need to go back to our meritocracy and not let the acts of some badly behaved people change who we are.
The thing is here. Even though he made a few points about possible confounders, his tone was so defensive and full of attacks on the Michigan authors that it made it hard to not view them as questionable. He took the observation that they might be indicative of systemic racism as a direct accusation of racism against him, and he also took a picture of himself. It was good for him and his wife to know that systemic racism can be maintained even if he is not a racist. He chose to respond with an editorial in a business journal instead of writing a letter.
The study was reported in a press release by Masimo. It was a retrospective analysis of Masimo laboratory data obtained from black and white volunteers in order to identify differences in Masimo pulse oximeter accuracy and bias between ethnic groups. I was interested in that. Is this study in the peer reviewed literature? It looks like it wasn't. I couldn't find it on PubMed if it was. The University of Michigan researchers are accused of publishing their work as a brief report in NEJM rather...incongruous.
Right here, I will say that I understand it. He felt attacked as being racist because his company is his life's work. Rather than asking what might account for the differences between his company's claimed data and the published reports, he went on the attack. Even though these observations weren't about him personally, Kiani thought they were about him.
I understand the urge to criticize how we do things in medicine as a personal accusation of racism. I learned to check that tendency. Being involved with a program at our cancer institute studying racial disparity in cancer care and outcomes as well as my stint on a statewide quality improvement initiative for breast cancer care is just some of the things I've been involved with. There are differences in outcomes in breast cancer. Even though there is a slightly lower incidence of breast cancer among Black women, age-adjusted breast-cancer mortality is about 40% higher among Black women than among non- Hispanic White women. There are a number of possible causes, including decreased access to screening, a higher rate of lack of health insurance, and a number of other factors. The disparity is beyond the scope of this post. There are differences in cancer outcomes.
There are stark differences in reproductive health care. In Missouri, black mothers died at four times the rate of white mothers during the year. Almost all of the deaths of pregnant women in Missouri are preventable. Blacks and American Indian or Alaska Native pregnant women have mortality rates that are over three and two times higher than the rate for White women. The Supreme Court's decision to make it easier to ban abortions in large swaths of the US is likely to make the disparity worse.
There is a list of these types of differences.
Science-based medicine can be used to study the causes of the disparity and technological fixes can be found.
In an optics lab at Brown University, PhD student Rutendo Jakachira explains how a pulse oximeter works.
“If you insert your finger in this groove, the LED at the top is sending light through your finger,” says Jakachira. The device can then calculate a patient’s oxygenation by figuring out how much of the light was absorbed by hemoglobin in the blood.
“That’s key to the problem being seen in people with dark skin, says Kimani Toussaint, a professor of electrical and computer engineering, biomedical engineering, and mechanical engineering at Brown University. “It’s assuming that the only absorber of the light energy is the hemoglobin.”
But in reality the skin pigmentation also absorbs the light, he says. And for people with darker skin, that can result in a reading from the pulse oximeter that overestimates the amount of oxygen in their blood.
Toussaint stands next to a table full of technology he hopes will solve the problem.
“I wouldn’t even call this a device yet,” he says.
Unlike current pulse oximeters, the not-quite-yet-a-device uses polarized light which isn’t absorbed by skin pigmentation. If it works correctly, Toussaint says they’ll partner with manufacturers to shrink it all down into a device that could be marketed.
And.
At Tufts University, Valencia Koomson is working on tackling this problem using a different approach.
Her device uses the same kind of light as currently available pulse oximeters do, but it includes technology that can measure a person’s skin tone (people with darker skin pigmentation have higher levels of melanin).
“We can send more light if there’s a higher level of melanin present, so that melanin doesn’t become a confounding factor that obscures our results,” says Koomson, who is an associate professor of electrical and computer engineering.
One example of racial disparity in medicine that science-based medicine needs to address is the case of pulse oximetry. It is an important one, and the magnitude of the disparity is not clear, but a technical fix could greatly mitigate it. The rest of the disparity in care is not easy to address.
It's one thing for certain. The process of researching the causes and solutions to the disparity will be slowed if we react to discussions of the disparity as though we are being personally attacked for being racist.