We thought about the origins of our blood. Blood cells originate from two different types of mother cells in a study using cellular "barcoding" in mice. The study was published in Nature on June 15.
"Historically, people have believed that most of our blood comes from a very small number of cells that eventually become blood stem cells," says Camargo, who is also a member of the Harvard Stem Cell Institute and a professor at Harvard University. A group of progenitor cells that don't come from stem cells were found. Most of the blood is made in fetal life until young adulthood, when it starts to decrease.
If the findings apply to humans, the researchers are going to follow up. New treatments for boosting aging people's immune systems could be influenced by these cells. They could help make bone marrow transplants more effective.
The codes for cellular phones.
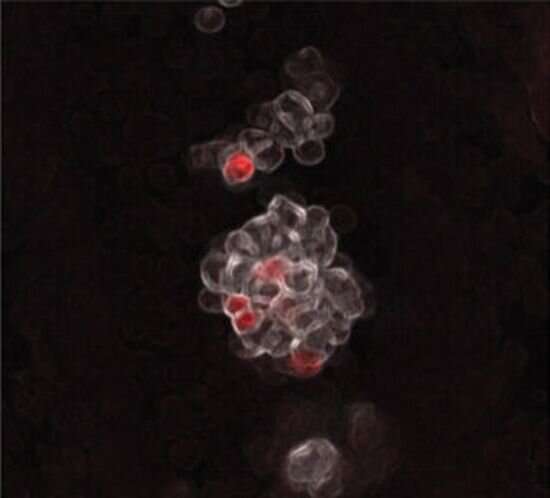
The barcoding technique developed by the team was documented in Cell. All the cells descended from them also carried the unique genetic sequence they were inserted into. The team was able to track the emergence of all the different types of blood cells.
"Now, people have these tools,TrademarkiaTrademarkiaTrademarkiaTrademarkiaTrademarkiaTrademarkiaTrademarkiaTrademarkiaTrademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,TrademarkiaTrademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia,Trademarkia The idea that stem cells give rise to all the blood cells was embedded in the field and no one tried to question it. Tracking what happened in mice gave us a glimpse of new biology.
The immune system is aging.
The researchers found that eMPPs are more abundant than blood stem cells in the presence of B cells and T cells. The decrease in eMPPs may explain why people's immunity weakens as they age.
"We're trying to understand why these cells peter out in middle age, which could potentially allow us to manipulate them with the goal of revitalizing the immune system."
In theory, there could be two ways to extend the life of eMPP cells, either through growth factors or immune signaling molecule, or by treating blood stem cells with gene therapy.
Blood cancers are not included.
The implications for better understanding and treatment of blood cancer are exciting. myeloid leukemias can affect myeloid blood cells. The leukemias may originate from blood stem cells and children's leukemias may come from eMPPs.
He says that they are looking at the effects of the mutations on blood stem cells and eMPPs in mice. If the leukemias that arise from these different cells of origin are different, we want to know.
Is it possible to improve bone marrow transplant?
There are two types of mother cells in the blood.
When we tried to do bone marrow transplants in mice, the eMPPs didn't last long. Adding a few genes could possibly be a better source for a bone marrow transplant. They are more common in younger marrow donors than blood stem cells, which may lead to better reconstitution of the immune system and fewer infections after the transplant.
More information: Fernando Camargo, Lifelong multilineage contribution by embryonic-born blood progenitors, Nature (2022). DOI: 10.1038/s41586-022-04804-z. www.nature.com/articles/s41586-022-04804-zSarah Bowling and her team created an engineered mouse line for simultaneous read out of genes in single cells. The journal is called 10.1016/j.cell.
Journal information: Nature , Cell